UNIQUE FEATURES
We are one of the first institutes to have the following facilities
NBI – Narrow-band imaging done for all regular endoscopies
it is useful for early detection of cancer and diagnosing Barrett’s esophagus.
RF Ablation – done for Barrett’s esophagus.
pH Manometry – 24-Hour pH/Impedance Reflux Monitoring is done for all patients of refractory GERD prior to surgery (Fundoplication).
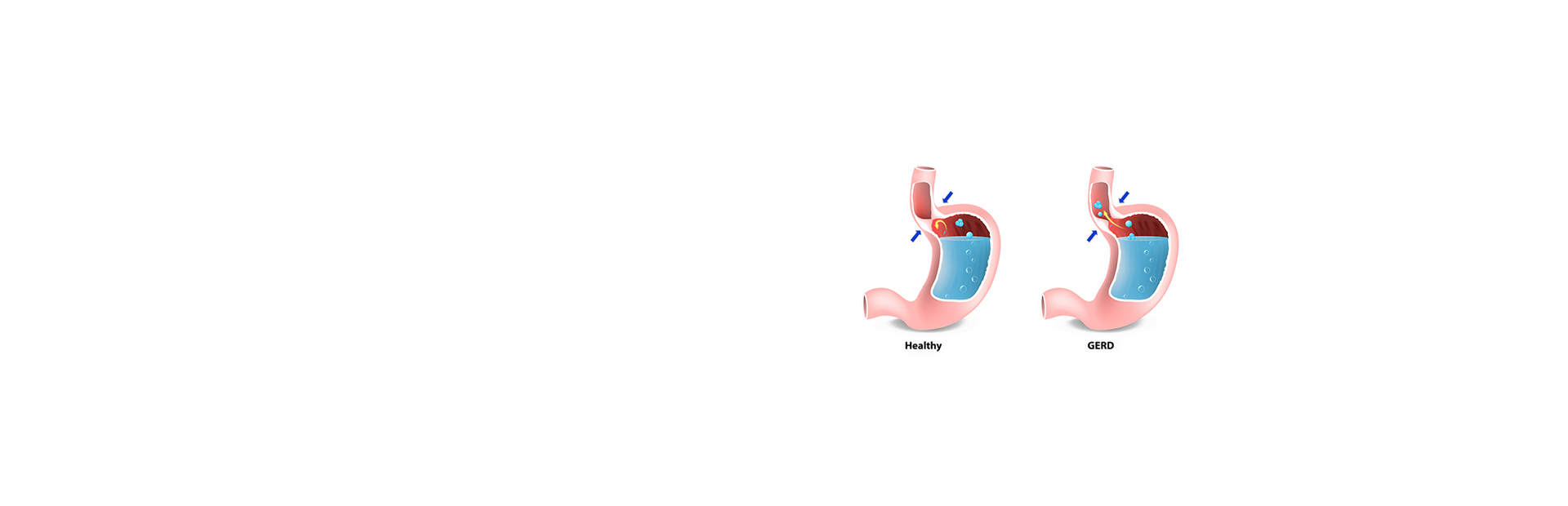
The oesophagus is a 40cm long muscular tube that joins our oral cavity with the stomach with the presence of a one-way valve at the lower end called “lower oesophageal sphincter.” Abnormal relaxation of this sphincter results in the regurgitation of gastric contents into oesophagus. Healthy individuals have an occasional reflux episode during the day, which is more common when they are awake. In an upright position, it gets cleared rapidly without causing acid-related injury to oesophageal mucosa.
Symptomatology
Typically GERD presents with heartburn, acid regurgitation, and dysphagia. It may also present with atypical symptoms such as nausea, vomiting, postprandial fullness, chest pain, choking, chronic cough, hoarseness, and wheezing.

Factors Responsible for GERD:
Hiatus hernia – This is a condition in which a part of the upper stomach pushes up through the diaphragm into the chest cavity.
Obesity – People who are obese or overweight seem to have an increased risk of GERD. While the reasons for this are not well understood, it is thought to be related to increased pressure in the abdomen.
Pregnancy – Many women experience acid reflux during pregnancy. This usually resolves after delivery, and complications are rare.
Lifestyle factors – Some foods (including fatty foods, chocolate, and peppermint), caffeine, alcohol, and cigarette smoking can all cause acid reflux and GERD.
Improper and untimely meals, large meals, and lying down soon after meals also increase the risk of GERD.
Certain medications like oral steroids and Aspirin also can increase the risk.
Stages of GERD:
Stage 1: Mild
Patients experience mild symptoms of heartburn and regurgitation once or twice a month.
Stage 2: Moderate
In this category, patients experience more frequent symptoms of heartburn and regurgitation which require medical treatment with PPIs and if untreated these symptoms can affect daily routine.
Stage 3: Severe
Patients with severe GERD present with uncontrolled symptoms in spite of taking medications. These patients will need a surgical procedure like Nissen’s fundoplication to improve the quality of life.
Stage 4: Reflux induced complications or carcinoma oesophagus
Barret’s oesophagus is the complication of many years of untreated GERD. It is a precancerous condition that leads to carcinoma oesophagus if untreated. These patients will need surgical anti-reflux procedure and close follow up.
Approach to GERD Patient:
As most of the symptoms of GERD mimic underlying other GI disorders, cardiac and pulmonary conditions, it is always mandatory to rule out these premorbid conditions before treatment. Hence approach to a patient with GERD is multidisciplinary involving Gastro surgeon, Gastroenterologist, Cardiologist, Pulmonologist, and occasionally Psychiatrist. Usually patients present to Gastro surgeons because of various reasons. They are either failed medical therapy, relapse of symptoms after stoppage of medications, or to avoid taking medications for a long time. The patient will be asked thorough clinical history including duration and severity of symptoms, co-existing medical conditions, day-to-day routines, and food habits will be assessed to rule out precipitating factors.
Why Does it Need to be Diagnosed and Treated?
GERD has become increasingly prevalent in Asian countries in recent years. This is mainly due to the introduction of the western diet, sedentary lifestyle, and habits. The long duration of acid reflux in the oesophagus results in certain complications like Barret’s oesophagus, strictures, perforation, reflux induced pneumonia, and cancer of the oesophagus. To avoid these potential complications, it is very essential to treat this disease.
Diagnosis:
The diagnosis is based upon the patient’s symptomatology, imaging, and establishing the oesophageal exposure to gastric acid by 24hr pH manometry. As we have parallelly running medical gastroenterology team and state of the art equipment like Endoscope and Ambulatory 24hr pH manometry, the chances of successfully diagnosing and treating this condition are more. We can even provide cross-reference to Cardiologist and Pulmonologist if any coexisting illness is present.
Upper GI Endoscopy:
An endoscope is a specialised flexible tube instrument equipped with a video camera which will be passed from the mouth into the stomach to visualise the status of the internal lining of oesophagus, stomach, and duodenum. It is also possible to take a part of the tissues for biopsy during the procedure. The images are captured and documented for comparison as well as to assess the prognosis of the disease. The patients with GERD show a spectrum of findings ranging from ulcers to stricture formation due to acid exposure.
24hr Ambulatory pH Manometry
We take pride in announcing that ours was the first centre to set up Oesophageal Manometry in western Tamil Nadu.
It is a diagnostic tool to find out pH differences occurring in the lower part of oesophagus in patients with GERD symptoms. The primary components of pH manometry are 1) oesophageal catheter and 2) monitor. The catheter is passed through the patient’s nose into the lower oesophagus and it is plugged to monitor, which is fixed to the shoulder. The catheter is going to sense differences in pH each time acid refluxes into oesophagus and it will be recorded in the monitor. After 24 hours once the test completes, a detailed report will be obtained which gives a thorough conclusion about oesophageal motility, number of harmful acid refluxes into oesophagus and relaxation/contraction of LES.

Therapeutic Approach:
Once all the reports are ready, the patient will be called for detailed counselling. We will again ask for a brief clinical history and patients’ lifestyle, diet habits and medications to find out if there are any precipitating factors. The anxiety part will be taken care of by our Psychiatrist colleague.
1st line of management comprises improving generalised wellbeing, to avoid triggering factors and to avoid unnecessary medications.
Patients are advised to make certain lifestyle modifications like:
Elevate head end of the bed.
Decrease fat intake.
Stop smoking (tobacco inhibits saliva, stimulates gastric acid, relaxes LES).
Avoid recumbency 2 hours after eating.
Lose weight if obese.
Avoid foods that decrease LES pressure: Chocolate, alcohol, peppermint, coffee, maybe onions and garlic…etc.
Avoid foods that can irritate damaged oesophageal lining like Citrus juice, tomato juice, pepper…etc.
2nd line of management is reserved for moderate to severe symptoms and various medications are given to suppress acid production, to protect already formed ulcers from ongoing acid reflux, and to increase motility of the GI tract.
Proton pump inhibitors like Omeprazole, Pantoprazole, Rabeprazole, Esomeprazole…. etc. are given for 3 months.
Ulcer protective drugs like Sucralfate, Colloidal bismuth, Calcium alginate are given.
Various prokinetics like Itopride, Domperidone, Cisapride are given in combination with antacids.
3rd line of management is for patients who experience the symptoms in spite of lifestyle modifications, long term medication usage, and risk categories. Patients are counselled in detail regarding the procedure and surgical procedure is carefully chosen with respect to the 24hr Impedance Ph manometry. Few patients may need repeat endoscopy to document the presence of active or healed ulcers.
- Laparoscopic Nissen’s fundoplication is the most commonly performed procedure for GERD. In this procedure the upper part of the stomach is wrapped all around the lower part of the oesophagus to construct a valve-like structure. After the surgery the patient will be monitored in the recovery room and will be given adequate pain relief. On POD #1, an X-ray study will be done to confirm adequate narrowing of LES and gradually liquids and semisolids are allowed.
- Usually, patients will be discharged in 2-3 days, and they will be advised to continue the lifestyle medications, small frequent semi solid meals for a few days, and he/she will be called for follow up after 5-7 days.
Complications of GERD:
- Dysphagia – Long term uncontrolled GERD can cause erosive ulcers in the oesophagus which results in scarring and stricture formation leading to difficulty in swallowing.
- Bleeding – It can be due to erosive ulcers formed in the oesophagus due to recurrent reflux episodes.
- Recurrent throat irritations – Acid reflux is responsible for recurrent throat irritation.
- Recurrent chest infections – Reflux in the night hours can lead to aspiration into lungs thus leading to lung infections.
- Barret’s oesophagus – It is a precancerous condition characterized by a change in the lining epithelium of the lower end of the oesophagus. It leads to cancer of the oesophagus if left untreated.
- Carcinoma oesophagus – It is a cancer condition developing in the lower end of the oesophagus due to long term, uncontrolled GERD. Many lifestyle habits like smoking, excessive fat intake, and alcohol consumption add to the risk.
Reflux Clinic – FAQ
Other symptoms of GERD may include:
Pain in the upper abdomen
Chest pain
Difficulty swallowing (called dysphagia) or pain on swallowing (called odynophagia)
Persistent laryngitis/hoarseness (due to the acid irritating the vocal cords)
Persistent sore throat or cough
Sense of a lump in the throat
Nausea and/or vomiting
Halitosis